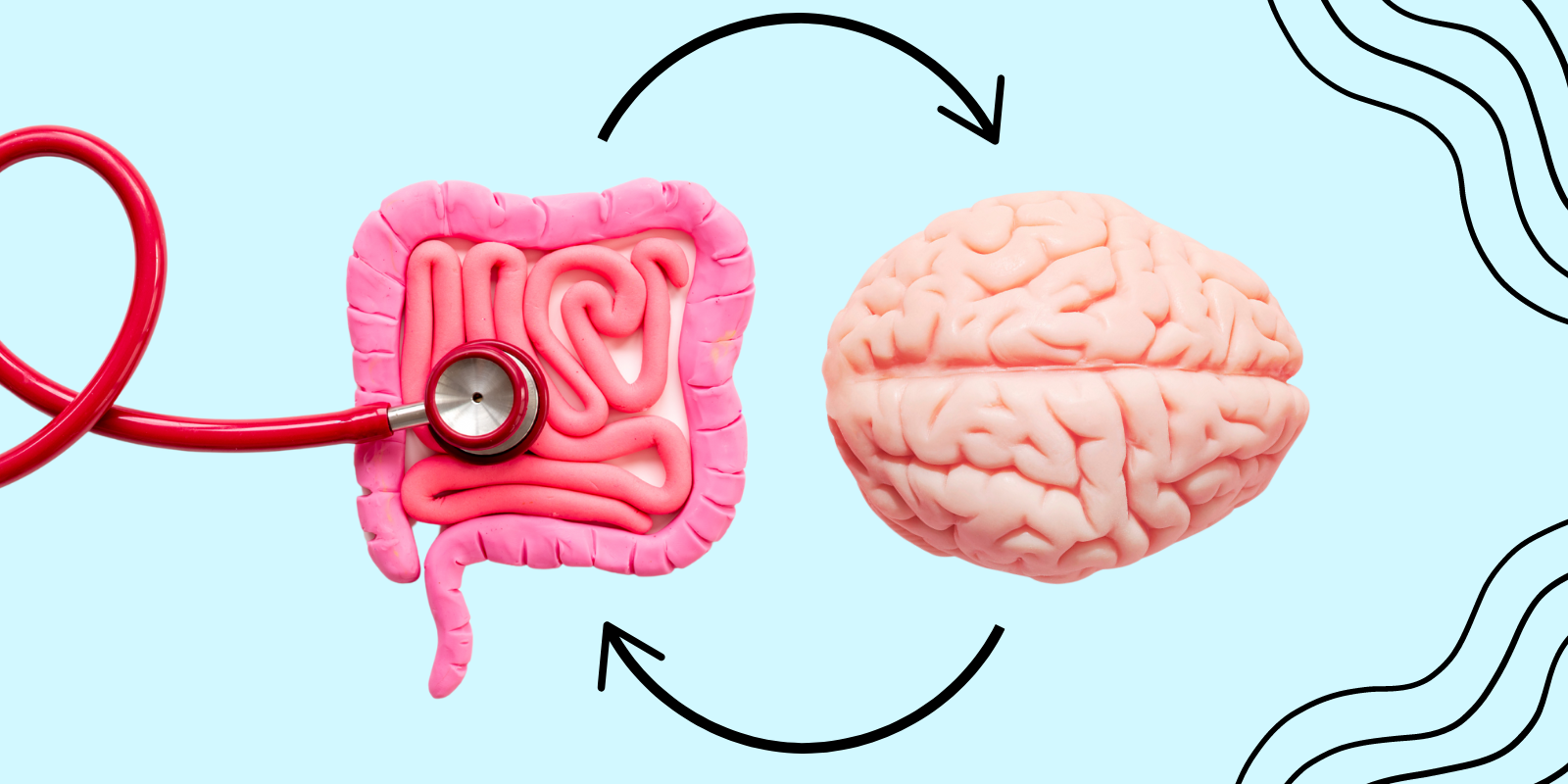
The connection between the gastrointestinal tract and the central nervous system has moved decisively from anecdotal observation—the familiar “gut feeling”—to a cornerstone of modern neurobiology and gastroenterology. The Gut-Brain Axis (GBA) is not a simple, one-way street; it represents a sophisticated, bidirectional communication system that intricately links the emotional and cognitive centers of the brain with the digestive functions of the gut. This communication network relies on a complex interchange of neural, hormonal, and immunological signals, profoundly influenced by the gut microbiome—the trillions of microorganisms residing in the intestines. A disruption in this axis, often starting with dysbiosis (an imbalance in the microbial community), can cascade into far-reaching consequences, affecting not only digestive health but also mood regulation, stress response, and even susceptibility to neurodegenerative conditions. Understanding the GBA requires appreciating the roles of the Vagus nerve, microbial metabolites, and the gut’s own extensive nervous system, revealing that the state of your digestion is, quite literally, inseparable from the state of your mind.
The Gut-Brain Axis Is Not a Simple, One-Way Street
The GBA is composed of several critical channels, operating simultaneously to ensure seamless communication. The Gut-Brain Axis is not a simple, one-way street; it is a complex, integrated circuit involving multiple signaling pathways. The most rapid and direct route is the Vagus nerve, the longest cranial nerve, which acts like a major highway. It carries signals from the brain down to the gut (modulating motility, secretion, and inflammation) and, crucially, sends far more information from the gut to the brain. This afferent signaling allows the brain to constantly monitor the gut’s physical and chemical status, including nutrient availability, local inflammation, and the composition of the microbial ecosystem. Beyond this neural highway, communication also relies on the release of hormones and neurotransmitters by the specialized cells lining the gut, which travel through the bloodstream to affect mood and cognition.
The Gut’s Own Extensive Nervous System, the Enteric Nervous System
The gastrointestinal tract possesses its own, comprehensive nervous network, earning it the moniker of the “second brain.” The gut’s own extensive nervous system, the Enteric Nervous System (ENS), is embedded within the walls of the esophagus, stomach, small intestine, and colon. The ENS operates largely independently, controlling vital digestive functions such as peristalsis (muscle contractions that move food), local blood flow, and the secretion of digestive juices. It is far more complex than a simple reflex arc, containing hundreds of millions of neurons—more than the spinal cord. While the ENS can manage the core mechanics of digestion autonomously, it is constantly modulated by the central nervous system (CNS) via the Vagus nerve, which explains why emotional states like stress or anxiety can immediately and physically disrupt gut motility, leading to symptoms like nausea or irritable bowel syndrome (IBS) flares.
The Trillions of Microorganisms Residing in the Intestines Profoundly Influence This Interplay
The complexity of the GBA is magnified exponentially by the presence of the microbiome. The trillions of microorganisms residing in the intestines profoundly influence this interplay through the generation of diverse metabolic byproducts. The relationship is symbiotic: the host provides food and shelter, and the microbes produce vital compounds. One of the most important classes of these compounds is short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate, which are produced when microbes ferment dietary fiber. SCFAs not only nourish the cells lining the gut but also cross the gut barrier and enter the circulation, where they can directly influence brain function and behavior, including regulating appetite and modulating the blood-brain barrier’s integrity. The composition of this microbial community is thus a critical determinant of the GBA’s overall health and function.
Microbial Metabolites Act As Crucial Signals to the Central Nervous System
The chemical language through which the microbiome talks to the brain is multifaceted. Microbial metabolites act as crucial signals to the Central Nervous System by influencing the production and availability of key neurotransmitters. Most notably, the gut is responsible for producing a significant proportion of the body’s serotonin, a neurotransmitter strongly associated with feelings of well-being, happiness, and appetite regulation. While this gut-derived serotonin does not typically cross the blood-brain barrier, it plays a vital role in gut motility and can modulate the activity of the Vagus nerve, indirectly influencing CNS function. Furthermore, gut microbes can produce other neuroactive compounds, including GABA (gamma-aminobutyric acid), which has calming, anti-anxiety effects, further cementing the gut’s status as a major biochemical communicator with the brain.
A Disruption in This Axis Can Cascade into Far-Reaching Consequences
The pathological consequences of chronic imbalance in the GBA are increasingly recognized in clinical practice. A disruption in this axis can cascade into far-reaching consequences, extending far beyond the digestive tract. Stress, poor diet, or antibiotic use can lead to dysbiosis, which compromises the gut barrier (leading to “leaky gut”) and triggers chronic, low-grade systemic inflammation. This inflammation, carried through the bloodstream, can signal the brain to alter mood states, making individuals more susceptible to anxiety and depression. Conversely, chronic psychological stress from the CNS can physically slow gut motility, reduce protective mucus production, and alter the microbiome, creating a vicious cycle of physical and psychological distress that traps conditions like IBS and functional dyspepsia.
The Gut Barrier’s Integrity Is a Cornerstone of Neurological Health
The physical wall of the intestine serves as a critical checkpoint, and its function is intimately linked to the health of the brain. The gut barrier’s integrity is a cornerstone of neurological health because it acts as the primary gatekeeper against systemic inflammation. When this barrier is compromised, inflammatory bacterial products, known as lipopolysaccharides (LPS), can enter the circulation. The presence of LPS triggers an immune response in the brain (neuroinflammation), which researchers now link to the pathogenesis of various mood disorders and potentially even neurodegenerative diseases like Parkinson’s and Alzheimer’s. Maintaining the tight junctions of the gut lining through diet and targeted supplements (like probiotics and prebiotics) is therefore seen as a proactive strategy for protecting the brain from peripheral inflammation.
The Communication Between the Gut and the Brain Is Not Static
The relationship between the GBA and external factors makes it highly dynamic and responsive. The communication between the gut and the brain is not static; it is continuously shaped by diet, stress levels, exercise, and pharmaceutical intake. For example, a single night of poor sleep or a high-stress event can acutely alter the permeability of the gut lining and change the composition of the microbiome. Similarly, dietary changes—such as introducing a high-fiber, diverse plant-based regimen—can lead to measurable shifts in microbial diversity and metabolite production within days. This dynamism means that the GBA offers a powerful, accessible target for lifestyle intervention; simple, consistent changes to diet and stress management can rapidly translate into improvements in both digestive comfort and mental well-being.
Diet Is the Single Most Powerful Lever for Modulating the Axis
Given the microbiome’s central role, it follows that the most effective, non-invasive tool for influencing the GBA is what we consume. Diet is the single most powerful lever for modulating the axis, providing the necessary substrates to encourage a diverse, balanced, and beneficial microbial community. A diet rich in fermentable fiber, low in highly processed ingredients, and adequate in anti-inflammatory omega-3 fatty acids creates an environment conducive to the production of beneficial SCFAs and protective mucus. Targeted use of probiotics, particularly strains demonstrated to influence neurological function (known as psychobiotics), can be used to introduce specific bacteria to modulate GABA or serotonin pathways, offering a potential adjunct therapy for mood disorders rooted in gut dysbiosis.
The GBA Offers a Powerful New Target for Treating Psychological Distress
The bidirectional nature of the GBA has fundamentally changed the landscape of mental health research. The GBA offers a powerful new target for treating psychological distress that previously relied solely on central nervous system intervention. Instead of exclusively targeting the brain with psychoactive medications, researchers are now exploring interventions that begin in the gut. These include specialized diets, fecal microbiota transplantation (FMT), and psychobiotic supplementation aimed at resetting the microbial balance. This emerging field recognizes that managing anxiety, depression, and stress may be achieved by calming the immunological and hormonal signals originating in the gut, thereby reducing the chronic inflammatory signaling that promotes negative emotional states in the brain.
This Holistic View Moves Beyond Symptom Management
The ultimate takeaway from this research is a shift in perspective on human health and disease. This holistic view moves beyond symptom management to address the root systemic imbalance. By recognizing the physical connection between the gut and the brain, practitioners are encouraged to screen patients presenting with mood disorders for underlying gastrointestinal issues, and vice versa. This integrative approach acknowledges that chronic digestive complaints (like chronic constipation or bloating) are frequently intertwined with psychological factors (like anxiety or hyper-vigilance). Treating both ends of the axis concurrently—with a combination of psychotherapy, stress reduction, and targeted dietary/microbial modulation—leads to more sustainable and comprehensive health outcomes than addressing either system in isolation.
